I am a headache specialist and so I receive many questions, through SBM, NeuroLogica or listeners of the Skeptic’s Guide to the Universe, about how to best treat headaches, or about a specific, often unusual, treatment. Migraines and severe headaches are very common. According to the latest statistics:
14.2% of US adults 18 or older reported having migraine or severe headache in the previous 3 months in the 2012 NHIS. The overall age-adjusted 3-month prevalence of migraine in females was 19.1% and in males 9.0%, but varied substantially depending on age. The prevalence of migraine was highest in females 18-44, where the 3-month prevalence of migraine or severe headache was 23.5%.
That means about 28 million Americans suffer from migraines. Percentages do vary from continent to continent, but not dramatically. Migraine, therefore, is a huge burden. Headaches can be debilitating when severe, and so also are a major source of lost productivity.
This will be a two-part series reviewing some of the options for treating migraines, focusing on science-based treatments in part I, and non-science-based treatments in part II. None of this is intended to give specific medical advice for any individual. If you have severe headaches you should consult your physician. I will simply be reviewing the evidence for various options, focusing on migraine specifically.
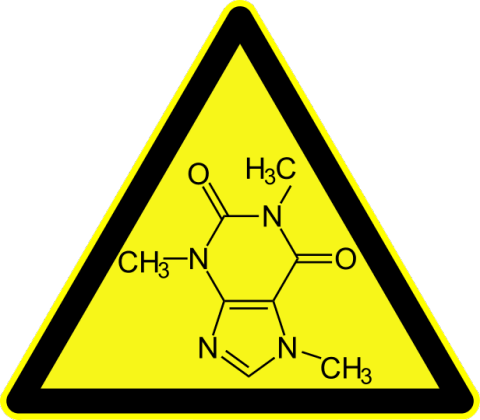
Caffeine, a common trigger for migraines and headaches
Lifestyle factors
The first step in approaching chronic headaches is to identify any lifestyle factors that may be playing a role and can be optimized. The more frequent and severe the migraine, the more important this becomes. This does not necessarily mean that the lifestyle factor is causing the headaches (although it may) but rather it could be triggering headaches or just making them more frequent.
Perhaps the most common trigger I encounter is caffeine. It is possible to have a pure caffeine-withdrawal headache, or for caffeine or caffeine withdrawal to trigger a migraine or increase its frequency. Eliminating caffeine should always be step 1 for reducing a chronic headache. Caffeine is present in coffee, tea, cola and other soft drinks, and chocolate. The recommendation for migraine sufferers is no more than 1 8oz beverage with caffeine per day (that giant 32oz coffee is actually 4 cups), although I prefer for my patients to completely eliminate caffeine when we are trying to maximally-remove triggers. Decaffeinated products should have about 3% of the caffeine normally present, but studies looking at actual products found that some can contain as much as 15% caffeine, enough to be physiologically significant if you drink a lot of decaf coffee.
Clues that caffeine may be playing a role are that your headaches occur in the evening or upon awakening, when it has been the longest since your last dose of caffeine. Weekend headaches, when people sleep in and delay their caffeine drinking, may also be a caffeine-withdrawal pattern. Also, if taking caffeine treats the headache, you are likely treating caffeine withdrawal. It takes at least seven days for the caffeine withdrawal symptoms to go away, but may take several weeks. I like to give my patients a caffeine-free trial for two to three months at least to see what their baseline headaches are like off caffeine.
There are many other possible triggers – red wine or other alcohol, foods with nitrates, aged cheese and deli meats, pickles, and MSG are common. (Studies of MSG do not show any consistent effects, but if an individual finds it is a consistent trigger it’s reasonable to avoid it.) The best way to determine what your triggers are is to keep a headache diary. There are now plenty of apps to help you do this.
Other lifestyle factors include getting regular sleep. Sleep deprivation can trigger a headache or worsen overall headaches. Optimizing sleep is therefore essential, and if you have a full sleep disorder then seek medical attention for that underlying problem. Too often patients don’t make the connection between their poor sleep and other symptoms, and don’t realize that a chronic sleep disorder is a medical condition that requires attention.
Keeping well hydrated and not skipping meals is also important. Don’t overdo the hydration, but make sure you keep well hydrated, especially on long flights, when it is hot or dry, at high altitudes, or when engaging in physical activity. Regular moderate exercise may also help manage migraines.
Nutrition
Several nutritional factors have been linked to migraines or may help with treatment. There is evidence that patients suffering from migraines have a greater chance of being low in magnesium. Evidence for a benefit from routine magnesium supplementation is encouraging but limited at this time, so it is not possible to make a strong recommendation for it. Some experts recommend getting more magnesium in the diet rather than using supplements. I tend to check magnesium levels and supplement when low.
Vitamin B2 (riboflavin) may help reduce migraines, but evidence is limited. The same is true for coenzyme Q10, which has the added disadvantage of being expensive. There is no evidence that a general multivitamin is helpful. As is often the case, the best advice is to have a well-rounded diet. Specific supplements as above may be considered in patients who cannot use medication or want to avoid it, but I have never seen a dramatic response to nutritional interventions alone in severe migraine.
OTC medication
Most migraine patients do not seek medical attention and treat themselves with over-the-counter medication. This is reasonable and there are several good options. NSAIDS (aspirin-like drugs) are a reasonable first line treatment for migraines. They are both anti-inflammatory and analgesic (pain killing). Migraine has an inflammatory component and so the anti-inflammatories may be especially helpful. Acetaminophen, which is not anti-inflammatory, is still effective in many patients.
Taking a medication at the onset of a headache is called an “abortive remedy.” To optimize abortive treatment, take it as soon as you know you are getting a headache. If you have an aura or warning before the headache, take it then. Don’t wait. There is literally a window of opportunity to effectively abort a migraine – don’t miss it. This means having your medication with you at all times. Take the medication with additional hydration. Avoid bright light, loud noise, or anything else that worsens your migraines until it resolves.
Using medication in this way up to once or twice a week should not be an issue for most people (again, consult your physician if you have other chronic conditions that need to be taken into consideration, such as stomach, kidney, or liver problems). If you have more than one to two headaches per week, you probably should be consulting your physician. Taking medication more frequently than that on a long-term basis can cause ulcers or kidney problems for NSAIDS, or liver problems with acetaminophen.
Also, taking any pain medication more than 1-2 times per week can cause what are called rebound headaches, or a medication overuse syndrome. In such cases headaches become more and more frequent, they can become daily, and result in dependence on the pain medication. Definitely seek medical attention before increasing your headache treatments to this extent. It is easier to prevent than to treat a medication overuse syndrome.
Prescription medication
I am not going to give a detailed description of the use of prescription medications for migraine. By definition, you will be seeking medical attention for prescription management. Such a long discussion is also beyond the scope of this article. For professionals there are already thorough reviews out there. The American Headache Society, for example, publishes excellent reviews. Here is a review of the evidence for acute treatment of migraines, and here is one for migraine prevention.
It is good to know, however, what kinds of options are available.
Your doctor can give you prescription strength and other formulations of NSAIDs to optimize their benefit. In addition, there is a class of medications called triptans which can be very effective in aborting migraines, either alone or in combination with NSAIDs.
If you have nausea with your headache to any extent, then treating the nausea can be a very effective method for treating the overall migraine.
There are also many options for migraine preventive therapy. These are medications taken every day in order to reduce the number and severity of migraines or make them more amenable to abortive treatment. These therapies should be carefully individualized, mostly by their side effect profile.
Botulinum toxin is also an approved therapy for migraine prevention in the US. This is given as a series of injections every three months, which some patients may prefer to a daily medication. This can be a very effective option in some patients.
About 60% of women with migraines are responsive to changes in their hormonal status. It may be possible to manage migraines by targeting prevention at high risk times during their cycle, or by adjusting their hormonal therapy.
For many patients who have headaches that are beyond self-treatment, your primary care doctor should be your first stop. They can decide whether or not to refer you to a specialist, which is usually a general neurologist. There are also neurologists who are specialized in headache medicine, and there is now board certification for this specialty. Finally there are some multi-disciplinary headache clinics for the most severe patients.
Conclusion
The purpose of this quick overview is to help individuals with chronic headaches optimize their self-treatment, and have a basic understanding of the options available from health professionals, including the range of experts that are available.
To reiterate – this cannot substitute for specific medical advice, which has to be individualized. Defer to your doctor if you have any questions about your headaches. Also, it is appropriate to seek medical attention for any severe headache syndrome, worsening headaches, new headaches, headaches that are difficult to treat, or any headaches associated with other worrisome symptoms. Acute severe headaches should be seen urgently in an emergency setting.
Next week I will review more speculative treatments for headaches, or those that specifically lack plausibility and/or evidence to support them.

